Bone Density Test: Purpose, Types and T-score Interpretation
A bone density test or a bone mineral density test determines whether you have a systemic skeletal disorder that causes bones to become weak and brittle, known as Osteoporosis. When you have Osteoporosis, your bones are more likely to break. It is a silent skeletal disorder, which means you may not experience any symptoms. Without a bone density test, you won’t be able to realise whether you have this condition until any of your bone breaks.
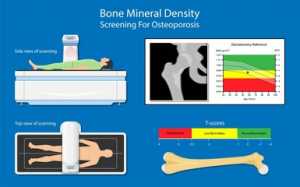
The bone density test estimates how many grams of calcium and other bone minerals are packed into each bone segment, using x-rays. Bones that are generally tested are in the hip, spine, and at times, the forearm.
If you have more bone minerals, the better it is, since it indicates that your bones are denser, stronger and less susceptible to break. Whereas, if you have fewer bone minerals, then your bone is more likely to break in a fall.
Why is the Bone Density Test Done?
Your doctor may order this test to:
- Determine drop in bone density before your bone breaks.
- Ascertain your risk of fractures
- Monitor treatment for Osteoporosis
- Confirm Osteoporosis diagnosis
Osteoporosis is more common in women than men because women have thinner and smaller bones, but the condition can also affect men as well. Your chances of developing Osteoporosis increases as you age. No matter your gender or age, your doctor may order this test if you have:
Lost height: Osteoporosis is one of the causes of compression fracture. If you have lost a minimum of 4 cm or 1.6 inches, then you may have compression fractures in your spine.
Fractured a bone: Fragility fracture occurs when your bone becomes brittle, which results in fracture much more easily than expected. A strong sneeze or cough can also cause Fragility fractures.
Received a transplant: You have a higher risk of developing Osteoporosis if you had a bone marrow or organ transplant. This is because anti-rejection medications also interrupt bone rebuilding.
Taken certain medications: Use of steroid medications such as Prednisone, Cortisone, Dexamethasone interrupt bone rebuilding. This results in Osteoporosis.
Had a drop in hormone levels: Besides the natural hormonal drop following the menopause, there is also a drop in women’s estrogen levels while they’re undergoing cancer treatment. Also, in men, certain treatments for prostate cancer may decrease the level of testosterone. A drop in sex hormone levels makes the bone weak.
Your doctor may also recommend having this test if you are:
- A woman aged 65 or above
- A postmenopausal woman aged 50 or above
- A woman below the age of 65 years, who already has been through menopause, and has a high risk of developing Osteoporosis.
- A man aged 50 years or above having Osteoporosis risk factors
- Having a more hunched posture
- Having back pain without any cause
- Your menstruation is either irregular or has ceased even if you’re not menopausal or pregnant.

What Are the Preparations Required Prior to the Test?
Bone density tests are painless and only lasts for less than 15 minutes. You may not need any preparations virtually. But make sure that you inform your doctor if you have undergone a barium exam, nuclear medicine test or had contrast material injected for a CT scan recently. Contrast may affect the test results.
For at least 24 hours prior to the test, you should avoid taking calcium supplements.
Wear comfortable and loose clothes, and choose not to wear clothes having buttons, belts, or zips. Make sure that you don’t have any metal objects such as change, money clips or keys in your pockets.
What is the Test Procedure?
Bone density tests are often done on bones more susceptible to break, such as:
- Bones in the forearm
- Bones in the lower lower back
- Narrow femoral neck
The two different types of Bone density tests are:
Central DXA– Central Dual-energy X-ray Absorptiometry, measures bone density at your hip bones and spine. Even though central DXA costs more, it tends to be more accurate.
For these diagnostic tests, you will be asked to lie down on a padded platform, and a mechanical arm moves over your body. It sends X-rays through your body and creates an image of your skeleton. The amount of radiation that you expose is much low in contrast to the amount of X-ray during a chest x-ray. The central DXA typically lasts about 10 to 30 minutes. The image will be sent to an expert who reads the result.
Peripheral Test– A Peripheral test checks the bone density of your heel, finger and wrist. Even though the test is cheaper, it is inaccurate since it doesn’t examine the spine or hips. Peripheral tests are screening tests for those who have a greater chance of developing Osteoporosis. The test is also administered in obese people, who won’t be able to undergo central DXA, due to weight limitations.
A small, movable machine is used to check bone density in the bones of your heel, finger and wrist. The instrument often used for the peripheral test is known as the peripheral devices.

What Do the Results Indicate?
Your results are expressed in two numbers- T-score and Z-score.
T-score: It compares the bone density of a healthy person of the same gender, with that of your bone density. The score can be normal, below normal, or level that can be a sign of Osteoporosis.
|
T-score |
What your T-score indicates |
|
-1.0 and above |
Normal BMD |
|
-1.0 to -2.5 |
Low BMD, and it may lead to Osteoporosis |
| -2.5 and below |
Osteoporosis |
Z Score: It compares your bone mass with that of other people of your same gender, age and size. If your Z-score is less than -2.0, it indicates that when compared to other people of your age, you have abnormal bone loss is because of something other than ageing.
Frequently Asked Questions
How often should I take this test?
You’re expected to take this test every 1 or 2 years if you’re under medication for Osteoporosis. Your doctor may recommend taking this test, even if you’re not having this condition, particularly women during or after menopause.
When should I have my follow-up bone density test done?
A follow-up bone density test should be taken every two years. But your doctor may suggest testing more often if you’re taking certain medications or currently have certain medical conditions. The follow-up test will be compared with that of the earlier tests to know what change has occurred.
If I have family members who have Osteoporosis, then do I also get Osteoporosis?
If Osteoporosis runs in your family, then you have an increased risk of developing Osteoporosis. The risk is more if your close relative, such as a parent or sibling has Osteoporosis. So you have to make sure that your diet includes calcium-rich food, and you’re engaged in a weight-bearing activity and should also avoid habits such as drinking alcohol and smoking.
Are bone density testing and bone scan the same?
No. Bone density tests are not the same as bone scans. They differ since bone scans are typically used to identify fractures, infections, inflammations cancer and other bone abnormalities, as well as normally need an injection of radioactive material beforehand.
I have a healthy diet and have no family history of Osteoporosis, but still, I have Osteoporosis. Why is it so?
There are various factors that can increase your chance of developing Osteoporosis. You’re more likely to develop Osteoporosis, if you’re having a thin build, and is postmenopausal. Your risk of getting Osteoporosis increases as you age. Besides that, certain medications and medical conditions also increase your chance of developing Osteoporosis.